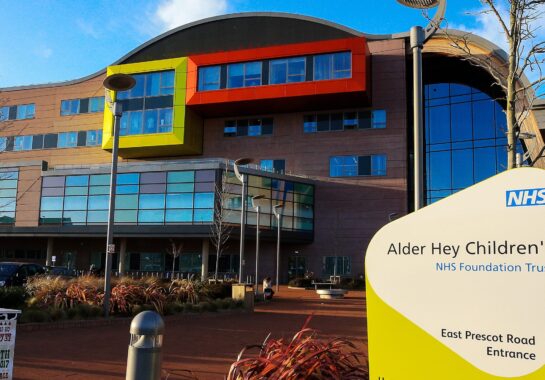
NHS
Liverpool-led study aims to predict final weeks of life for cancer patients
11 months ago

A ground-breaking research study, led by The Clatterbridge Cancer Centre (CCC) and the University of Liverpool (UoL), is pioneering a way to predict when cancer patients are approaching the end of life – marking the first study of its kind in the world.
The ‘Biology of Dying’ study, which has now secured £231,000 in funding from North West Cancer Research, aims to develop a tool that can accurately determine when a patient is in the final four weeks of life.
This revolutionary work could transform end-of-life care by giving patients and their families crucial time to prepare, while also enabling clinicians to provide more personalised and appropriate medical support.
Communication Medicine has published the research – led by and sponsored by The Clatterbridge Cancer Centre (CCC) and the University of Liverpool (UoL) – which found that lung cancer patients can have their risk of dying accurately predicted within the last four weeks of life.
The findings show that by analysing the urine of patients, it is possible with high accuracy to determine the likelihood of death, allowing patients and their families to better prepare and giving clinicians more information to enable better individualised patient care.

The ‘Biology of Dying’ study – led by Clatterbridge palliative care consultant Dr Seamus Coyle – recorded how metabolic changes taking place within the last 30 days of a patient dying can be measured to give a prediction of death, with accuracy increasing as the time of death nears.
Dr Coyle, an Honorary Senior Clinical Lecturer at UoL, said: “This is the first study of its kind in the world that aims to understand how we die from cancer, and how to accurately predict the last weeks and days of life.
“Despite thousands of years of medicine, we still do not know how we die from cancer, and predicting when someone dies of cancer is largely down to the judgement the clinical team rather than a medical test. This research changes that.

“We discovered there is a process to dying from cancer and it is associated with altered metabolism. We developed a urine test that predicts risk of death across multiple time points ranging from 4 weeks to the last days of life.”
Urine from 161 lung cancer patients were analysed to find potential biomarkers for dying. In a series of tests, 7 metabolites in the urine samples were shown to change to such an extent that significant predictions of death could be made, stratifying patients into having a low, medium and high risk of dying. The results within 30 days were shown to have “excellent” probability values.
“We are the only research team in the world to have demonstrated this and the new funding will help us to test our theories,” said Dr Coyle. “We discovered there is a process to dying from cancer and we now need to demonstrate our findings in a larger sample size.”

North West Cancer Research is funding an expansion of the study with a £231,000 grant and 1,327 urine samples will be collected from lung cancer patients in the last month of life from across the country.
Dr Coyle added: “Having knowledge of when a patient is due to die will improve end of life care and allows both patients and their loved ones to plan. It also gives clinicians better understanding so they can make more appropriate decisions about a patient’s medical care.”
Dr Gillian Heap, CCC’s Director of Research and Innovation Operations said: “This is very important world-leading research and we are delighted that this Clatterbridge-sponsored study is now to be expanded with this grant award. I’d like to thank Dr Coyle and his colleagues for their amazing research and our own Research Sponsorship Team which helped to secure this new funding.”
This research was made possible through the collaborative efforts of a dedicated team, Prof. Chris Probert (Royal Liverpool Hospital and University of Liverpool), and Dr. Elinor Chapman (University of Liverpool), among other valuable contributors.









 Subscribe
Subscribe Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us