Health & Fitness
Alder Hey surgeons use new technique to save life of boy with rare condition
6 months ago

Surgeons at Alder Hey Children’s Hospital have used a new technique to save the life of a toddler who was born with an extremely rare birth defect in what is thought to be a world first.
Conor O’Rourke, now three, was diagnosed with vein of galen malformation (VOGM) as a baby after a doctor raised concerns about the size of his head at an appointment for an unrelated issue.
The condition causes the veins and arteries in the brain to connect abnormally, increasing blood flow and leading to severe complications such as heart failure and brain damage, and death if undetected.
The toddler from Bolton is one of a rare subgroup of patients with VOGM which left him essentially untreatable.
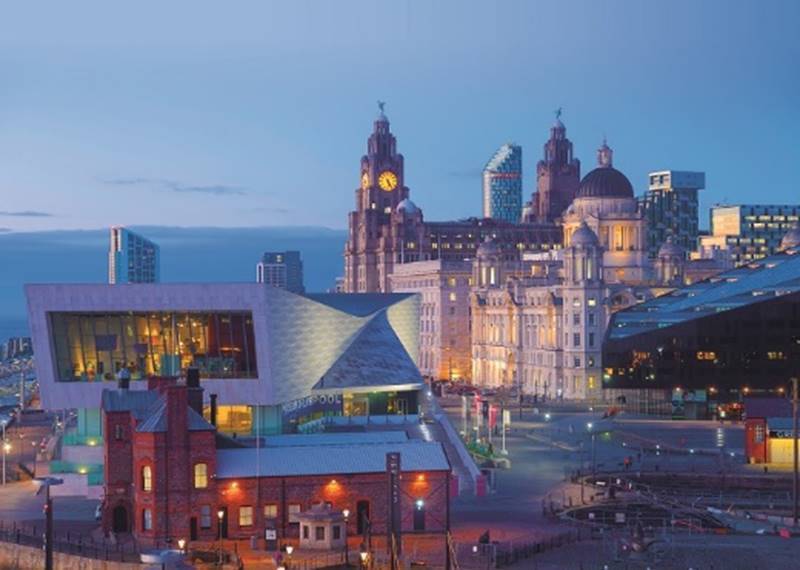
Specialists at Alder Hey Children’s Hospital in Liverpool performed the novel technique, which involved open surgery deemed “high risk”, in March.
Conor, who has since recovered well, would have deteriorated neurologically over a year or two without the operation, according to specialists.
His surgeon told the PA news agency the boy is now considered “99% cured” and has become a “different child”.
Conor was around eight or nine months old when his mum Lucy O’Rourke, 36, took him to an appointment with a consultant over an issue with his belly button.
However, while there, the doctor raised concerns about the size of her baby’s head.
Conor was eventually diagnosed with VOGM in March 2023, which his mum said was “terrifying”.
The condition causes arteries to connect directly to the vein of galen – a deep vein in the brain that drains blood from the brain back to the heart – rather than connecting to capillaries, which would slow down blood flow.
It affects roughly 10 to 12 babies in the UK every year.

Mrs O’Rourke said:
“I genuinely felt like I was living in a nightmare, and I felt like there was going to be a point where somebody was going to phone me and say, ‘sorry, we’ve mixed up the scans, this isn’t your child, we’ve got it wrong’, and we just felt completely helpless in that moment in time.
“We just cried and sat in silence for hours. We just didn’t know what to do with ourselves.”
The treatment for VOGM involves inserting a small, flexible tube called a catheter into the arteries, usually from the groin.
Medics use X-ray imaging to guide the tube through the body and into place, and then inject a glue-like substance to block off the artery.
In some cases, the same procedure can be performed by inserting the catheter into the veins. Conor had three of these operations in 2023.
Conor Mallucci, a consultant paediatric neurosurgeon at Alder Hey, said:
“Conor had already had those procedures, both from the artery and the vein, but after a while, in a rare subgroup of these patients, the veins block off and you can no longer get to the malformation.
“And you can’t get up there through the artery either, and so you’re left with an untreatable malformation that’s still supplying abnormal blood to the veins.”
When this happens, the jugular veins – a set of major blood vessels in the neck – block off.
“That’s rare to this condition, but it’s specific to this condition,” Mr Mallucci said.
“And when the jugular veins block off, which happened in Conor, the veins from the brain try and drain elsewhere.
“In his case, he had all these abnormal channels draining to his brain stem and spinal cord. And that results in swelling and damage, which is why he was deteriorating over time.”
Mrs O’Rourke told PA her son suffered a small stroke after his third operation in November 2023.
Around a year later, and after physiotherapy, the toddler’s family were told he was not in a position for more operations and they would scan him in 12 months’ time.
While his parents were initially “so happy” to have a year with no scans, they soon noticed their son was struggling.
Mrs O’Rourke said: “In early December, I started to notice that physically he was struggling, and he was limping quite a bit on his left leg.”
Mr Mallucci said, by this point, Conor was essentially “untreatable” and had “run out of all his options”.
“It’s a fight against time, and that happened quite early in Conor, which is why we had to come up with this alternative route,” he added.
“You couldn’t get into his head through the veins, because the jugular veins have blocked off, and you can’t block off through the artery any more.
“So that’s when we came up with our technique, which is to access the veins through open surgery beyond the blockage.”
The operation involved accessing the malformation through the skull to target the affected blood vessels.
Alder Hey is one of only two centres in the UK equipped to carry out this procedure on children.
The hospital has a state-of-the-art theatre with advanced imaging machinery, giving specialists real-time X-ray pictures of blood vessels during operations and allowing them to combine endovascular and open surgery.

The technique has never been performed at another hospital.
Mr Mallucci told PA: “Exposing these veins that were blocked at the jugular level is high risk.
“You lose blood. It’s a big operation, and to put a needle directly into one of those is a little bit hair raising, so we had to be very careful about that.”
Medics told Mrs O’Rourke her son would very tired after surgery and was expected to sleep for around a week and remain in hospital for up to six weeks.
However, Conor woke up soon after the operation asking for chips and the family were home after 10 days.
Mrs O’Rourke said: “I obviously went into mum mode and said ‘can we get some chips in here please?”
Speaking of Conor’s recovery, Mr Mallucci said: “He’s not only recovered well, everything that he had going bad was reversed.
“He’s become a different child, really, it’s like he’s suddenly been released.”
Mr Mallucci told PA Conor is considered “99% cured” and will not need any more operations.
Instead, he will have annual scans to monitor his brain and potentially have an angiogram – when a dye is injected into the bloodstream to allow doctors to capture images of blood vessels using X-ray – in around four to five years.
Mrs O’Rourke said: “No surgery now – unless we get broken arms or legs – but with something like that, we’re kind of like ‘bring it on’.
“As long as it’s not more brain surgery, then we’ll probably be able to cope with that.”
Specialists at Alder Hey have performed the new technique on two patients, including Conor, and have a third lined up.










 Subscribe
Subscribe Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us