NHS
NHS in the North West reveals plans to improve care and discharge times this Winter
3 years ago

Care ‘traffic control’ centres to speed up discharge, extended ambulance hours and extra beds are part of wide-ranging plans to prepare for winter announced by the NHS nationally yesterday.
The robust new measures, set out at the NHS England board meeting in Birmingham yesterday, will boost capacity and resilience across the NHS as well as building on the recent improvements in ambulance response times and A&E performance.
Winter preparations have been well underway since the publication of the NHS’s Urgent and Emergency Care Recovery Plan, with over 800 new ambulances set to be in place to deliver 3.4 million more ambulance road hours as well as 5,000 more sustainable hospital beds and hundreds of new virtual wards each month.
Nationally, the NHS will also be announcing a new incentive scheme to encourage local teams to ‘overachieve’ on performance and receive part of a £150m capital fund for 2024/25. Trusts will receive a greater proportion of funding if they achieve an average of 80% A&E four-hour performance in Q4 and have less than 5% of handovers over 30 minutes in the last half of this financial year.
With more than 12,000 patients every day in hospital despite being medically fit for discharge, a nationwide rollout of ‘care traffic control’ centres will provide one stop for staff to locate and co-ordinate the best and quickest discharge options for patients – either at home or into social or community care.
The centres will bring together teams from across NHS, social care, housing, and voluntary services in one place to help make live decisions and offer patients everything they need in one place.
Around a quarter of local areas currently offer this service 12 hours a day, seven days a week and this is set to expand to every area of the country by winter.
Drawing information from electronic patient records to track patients and link up with housing services, it is expected a third of patients could be discharged using this model by December.
NHS England North West Regional Medical Director Dr Michael Gregory said:
“Across the North West there are regularly 2,000 people in a hospital bed who no longer need the services only a hospital can provide, speeding up their discharge will help the ability for A&Es to see, treat and admit patients quickly.”
In the North West all Trusts already have Care Transfer hubs and a new service put in place at Wirral University Teaching Hospital NHS Foundation Trust earlier this year has already seen positive results.
After introducing a completely new way of working three months ago, in partnership with Wirral Council, NHS and voluntary sector organisations like Age Concern, the Trust has reduced the number of people in beds who are waiting to go home from 250 to 150 a day, freeing up 100 more beds at Arrowe Park and Clatterbridge hospitals.
“Doing things differently has really made a difference to speeding up getting patients out of hospital to a more appropriate place,” said Dr Gregory.
At the monthly board meeting, the NHS outlined how it is bracing for another winter facing the possibility of higher than usual levels of respiratory illness including Covid, flu and RSV. Australia, whose activity often predicts what the NHS in England is likely to see in winter, is experiencing one of the biggest flu seasons on record with children particularly affected, making up four in five of flu-related hospital admissions.
The use of Acute Respiratory Hubs – where patients can get urgent same-day face-to-face assessment for conditions like Covid, flu and RSV will also be expanded to be available in every part of the country.
Last winter in the North West additional acute respiratory infection hubs were created in 70 sites across the region, which were able to deliver an additional 95,000 appointments.
In Greater Manchester the MARIS (Manchester Acute Respiratory Infections Service) introduced same day assessments ensuring patients were seen more appropriately and improving the efficiency of the service.
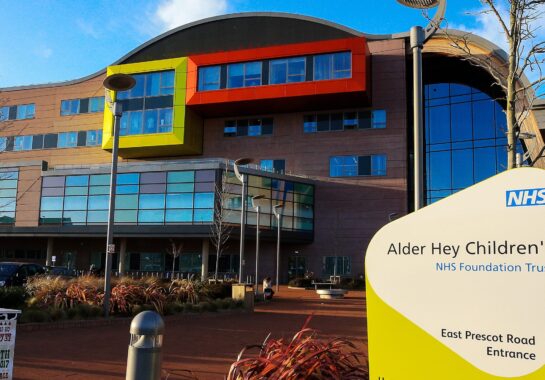
The East Lancashire Hub developed model which helped it deliver more than 9,000 appointments in one of the most deprived areas in the country. In Alder Hey Childrens Hospital a GP was placed in the A&E department triage for respiratory infection presentations.
With high levels of bed occupancy all year around, hospitals are putting more beds in place for patients and are on track to hit 5,000 additional ‘core’ permanent general and acute beds. Thanks to the efforts of the NHS, more than 99,000 core beds will be in place across the country by December 2023 – thousands more than last year, to boost resilience.
Since £250million of funding was announced in January to boost capacity and speed up discharge, local NHS areas are on track to create an additional 900 beds.
In the North West, plans are moving at pace to build a new modular ward at Lancashire Teaching Hospital NHS Foundation Trust, and create capacity by converting office space into ward space at East Lancashire Hospitals NHS Trust. These will create additional beds to treat patients this winter.
Earlier this month, the NHS announced its world-leading virtual ward programme would be expanding to children, with overall virtual wards bed numbers expected to hit our ambition of 10,000 by the end of September.

Virtual wards within the North West include services for frailty, acute respiratory infections, chronic obstructive pulmonary disease (COPD), heart failure and a number of paediatric virtual wards, which to date have cared for more than 16,000 patients since May 2022.
Local NHS teams will now focus on preparations across a variety of services including mental health, with plans to be put in place to strengthen ambulance response to mental health calls, continue to raise the profile of all-age 24/7 urgent mental health helplines and avoid long lengths of stay in mental health inpatient settings.
North West Ambulance Service also confirms that it will have 46 new emergency ambulances this year, growing the fleet by 28. They are also planning for seven new mental health response vehicles which will be operational by early 2024.
The ambulance service has also successfully piloted the Kia EV6 rapid response vehicle (RRV) and Mercedes eVito dedicated mental health resource as part of a national initiative. Following this, it has committed to replacing a further 52 RRVs with electric vehicles and engaging in an additional pilot. It has introduced electric vehicles for workshop and logistics teams and invested in over 90 charge points to support the infrastructure around this.
Dr Gregory added: “This winter we are planning early to ensure we have as much time as possible to prepare. We want patients to receive the right care, in the right place at the right time.”







 Subscribe
Subscribe Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us Follow Us
Follow Us